
Historically, mechanical complications following acute myocardial infarction have been associated with very high morbidity and mortality. Despite their incidence plummeted with the advent of acute reperfusion therapy, such as thrombolysis and percutaneous coronary intervention, contemporary data on the outcomes of patients who develop such ominous complications are scarce. CAUTION study (NCT03848429), a retrospective, international, multicenter study aimed at evaluating the survival and postoperative outcomes of patients undergoing cardiac surgery for post-infarction mechanical complications. The recent publications from this registry, CAUTION PMR study (DOI: 10.1093/ejcts/ezab469) and CAUTION VSR study (DOI: 10.1001/jamanetworkopen.2021.28309), revealed an early mortality of 24.8% and 40.4% for subjects underwent surgical treatment for post-infarction papillary muscle rupture (PMR) and VSR (ventricular septal rupture), respectively. In light of this, further efforts of the health community should be directed toward improving therapeutic measures in an attempt to improve in-hospital survival of these critical subgroups of patients. Furthermore, publications investigating the long-term outcomes of patients undergoing surgery for post-infarction mechanical complications are warranted.
Background
Historically, impaired glucose metabolism has been associated with early and late complicated clinical outcomes after cardiac surgery. Such a condition, however, is not specific to subjects with diabetes mellitus and involves larger patient population.
Methods
Databases were screened (January 2000-December 2020) to identify eligible articles; studies, which evaluated the association between preoperative metabolic status, as assessed by glycosylated hemoglobin (HbA1c) levels, and clinical outcomes were considered. The studies were stratified in thresholds by baseline HbA1c level (lower vs higher).
Results
Thirty studies, involving 34,650 patients, were included in the review. In a meta-analysis stratified by HbA1c levels, early mortality was numerically reduced in each threshold comparison and yielded the highest reductions occurred when <5.5% vs >5.5% HbA1c levels were compared [Risk Ratio (RR) 0.39, 95% Confidence Intervals (CIs) (0.18-0.84), P=0.02]. Comparing higher HbA1c threshold values yielded comparable results. Late mortality was reduced with lower levels of HbA1c as well. Low pre-op HbA1c was associated with lowest risk of sternal wound infections [RR 0.50, 95% CI (0.32-0.80), p=0.003 and RR 0.53, 95% CI (0.39-0.70), p<0.0001] for comparisons of <7.5% vs >7.5% and <7.0% vs >7.0% HbA1c thresholds, respectively. Additionally, levels of HbA1c lower than 7% were associated with reduced hospital stay, lower risk of stroke/transient ischemic attack [RR 0.53, 95% CI (0.39-0.70), p<0.0001 and acute kidney injury: RR 0.65, 95% CI (0.54-0.79), p<0.0001].
Conclusions
Lower levels of HbA1c in patients undergoing cardiac surgery are associated with lower risk of early- and late mortality, as well as in the incidence of postoperative AKI, neurological complications, and wound infection, as compared to higher levels.; Keywords: diabetes mellitus; cardiac surgery; glycosylated hemoglobin; coronary artery bypass grafting.
full text (.PDF) available at JTCVS website
accompanying editorial (Breaking the Perioperative Glucose Control Barrier Is Like Breaking the Sound Barrier – It Takes a Team!) by Victor A. Ferraris
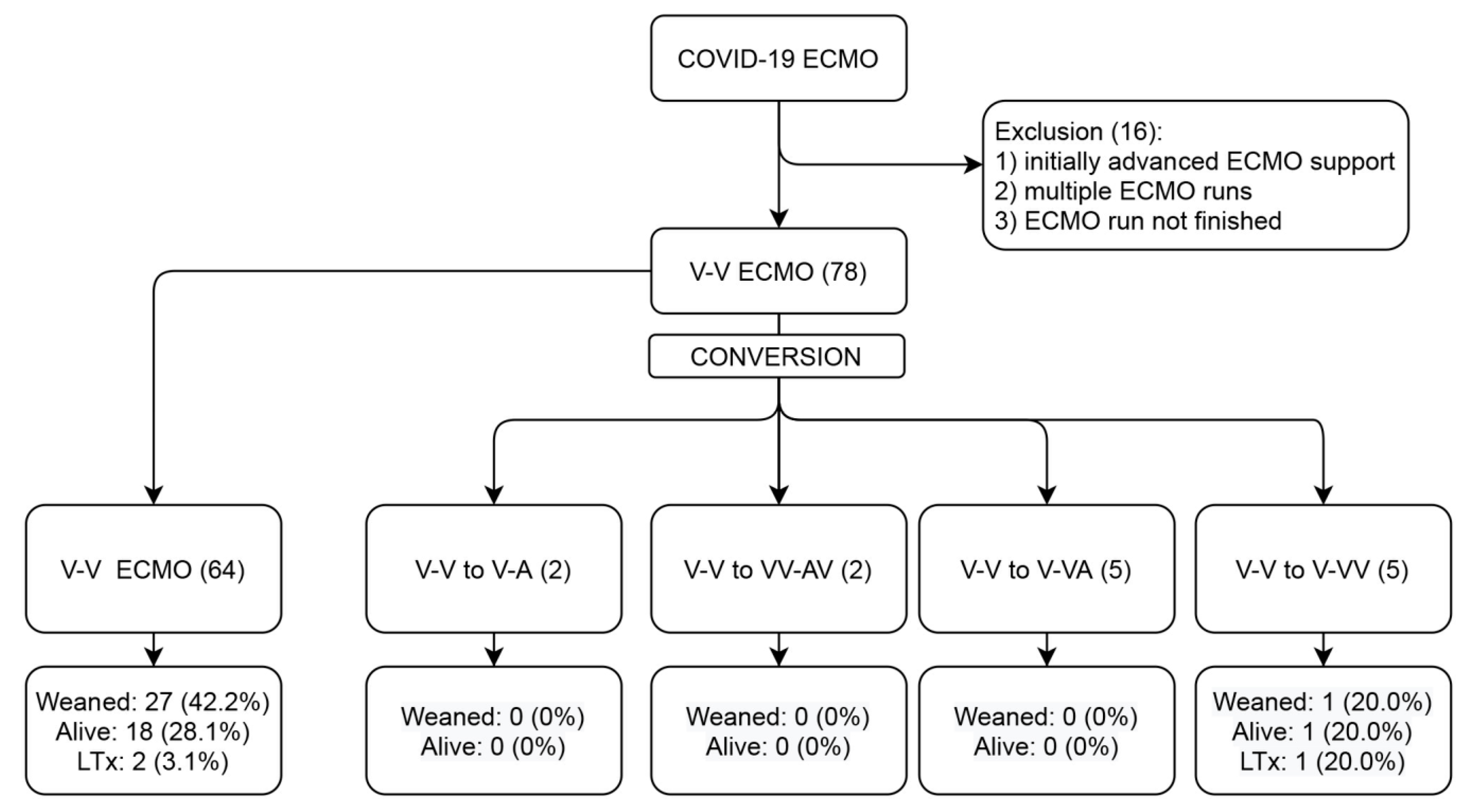
In SARS-CoV-2 patients with severe acute respiratory distress syndrome (ARDS), Veno-Venous Extracorporeal Membrane Oxygenation (V-V ECMO) was shown to provide valuable treatment with reasonable survival in large multi-centre investigations. However, in some patients, conversion to modified ECMO support forms may be needed. In this single-centre retrospective registry, all consecutive patients receiving V-V ECMO between 1 March 2020 to 1 May 2021 were included and analysed. The patient cohort was divided into two groups: those who remained on V-V ECMO and those who required conversion to other modalities. Seventy-eight patients were included, with fourteen cases (18%) requiring conversions to veno-arterial (V-A) or hybrid ECMO. The reasons for the ECMO mode configuration change were inadequate drainage (35.7%), inadequate perfusion (14.3%), myocardial infarction (7.1%), hypovolemic shock (14.3%), cardiogenic shock (14.3%) and septic shock (7.1%). In multivariable analysis, the use of dobutamine (p = 0.007) and a shorter ICU duration (p = 0.047) predicted the conversion. The 30-day mortality was higher in converted patients (log-rank p = 0.029). Overall, only 19 patients (24.4%) survived to discharge or lung transplantation. Adverse events were more common after conversion and included renal, cardiovascular and ECMO-circuit complications. Conversion itself was not associated with mortality in the multivariable analysis. In conclusion, as many as 18% of patients undergoing V-V ECMO for COVID-19 ARDS may require conversion to advanced ECMO support.
full text (.PDF) available at Membranes website
